Frozen Shoulder
Frozen shoulder, or adhesive capsulitis, is a condition characterized by stiffness, pain, and limited range of motion in the shoulder joint. It occurs when the capsule of connective tissue surrounding the shoulder thickens and tightens, restricting movement. Typically affecting people aged 40-60, it’s more common in women and those with diabetes, thyroid disorders, or prolonged immobility (e.g., post-surgery or injury). Other risk factors include heart disease, stroke, or autoimmune conditions, though the exact cause often remains unclear.
The condition progresses through three stages. The freezing stage involves increasing pain and gradual loss of motion, lasting weeks to months. In the frozen stage, pain may subside, but stiffness peaks, severely limiting activities like reaching overhead or behind the back, often for 4-12 months. The thawing stage sees gradual improvement in mobility, though full recovery can take 1-3 years. Symptoms vary in intensity, with night pain disrupting sleep in early stages.

Self-management plays a key role. Consistent, guided exercises, heat therapy, and posture awareness aid recovery, while avoiding overuse prevents setbacks. Though frozen shoulder often resolves over time, some experience lingering stiffness. Early intervention and adherence to therapy improve outcomes. Awareness of risk factors, like diabetes control or avoiding prolonged immobility, can reduce incidence. With patience and proper care, most regain near-normal shoulder function, reclaiming daily ease.
Frozen shoulder, also known as adhesive capsulitis, is a condition characterized by stiffness, pain, and limited range of motion in the shoulder joint. It typically develops gradually and progresses through stages—freezing, frozen, and thawing. Causes include injury, surgery, or prolonged immobility, though it can also occur without a clear trigger. Treatment involves physical therapy, pain management, anti-inflammatory medications, and sometimes corticosteroid injections. Most people recover over time with consistent therapy and care.
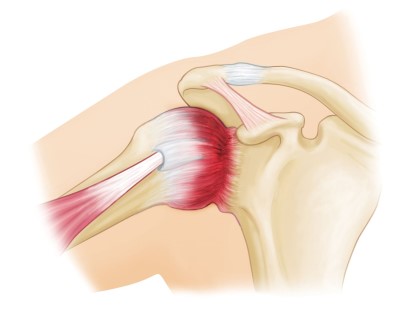
Diagnosis relies on medical history and physical exams assessing range of motion. Imaging like X-rays or MRIs may rule out arthritis or rotator cuff issues. Treatment aims to reduce pain and restore function. Conservative approaches include physical therapy with gentle stretching exercises to improve mobility and strengthen muscles. Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections help manage pain and inflammation. In persistent cases, procedures like hydrodilatation (injecting fluid to stretch the capsule) or arthroscopic surgery to release adhesions may be considered.